Understanding Scleroderma Rash: What Skin Changes To Look For
When you hear about scleroderma, your thoughts might first turn to changes in the skin. This condition, after all, very often makes its presence known through visible alterations on the body's largest organ. The term "scleroderma rash" might not describe a typical itchy, red breakout, but it points to the unique and sometimes striking ways this disease can affect your skin. It’s a topic many people are curious about, and for good reason, too it's almost the first thing people notice.
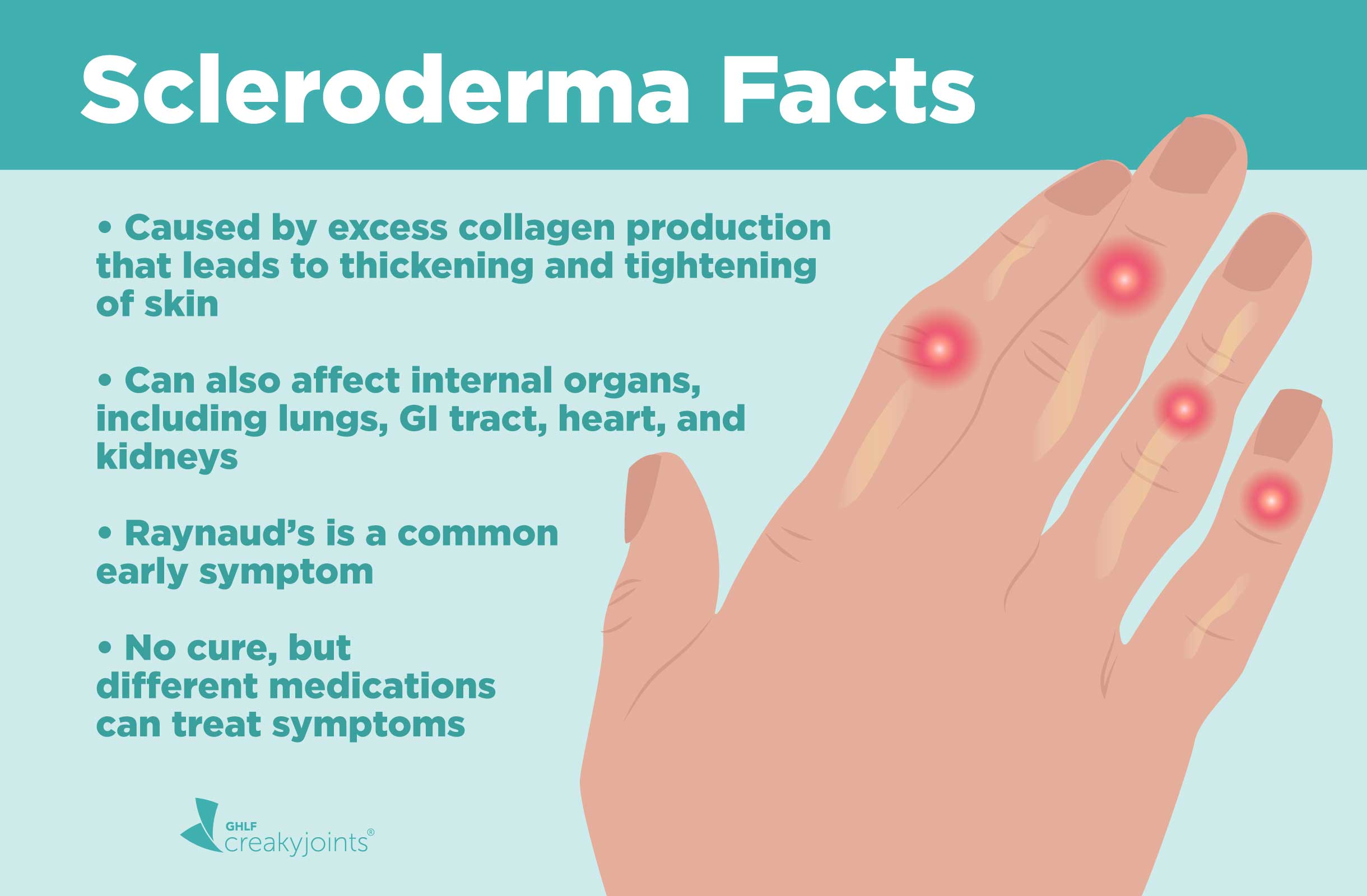
Scleroderma is a chronic condition that causes the body to produce tissue that's thicker than it should be. It's considered an autoimmune disease, which means your body's immune system, which is that meant to protect you, mistakenly starts attacking its own healthy tissues. This can lead to various effects, with skin changes being among the most common and noticeable, as a matter of fact.
This article aims to shed some light on the diverse ways scleroderma can show up on your skin. We will explore what these skin changes look like, why they happen, and what you can do to manage them. Understanding these aspects can help you feel more in control, and really, that's what we want to help you achieve.
Table of Contents
- What is Scleroderma, Anyway?
- The Many Faces of Scleroderma Skin Changes
- Why Does Scleroderma Affect the Skin?
- Localized vs. Systemic Scleroderma: Skin Differences
- Getting a Diagnosis: When to See a Doctor
- Living with Scleroderma Skin Changes: Tips and Support
- The Future of Scleroderma Research and Treatment
- Frequently Asked Questions About Scleroderma Skin
- Seeking Help and Support
What is Scleroderma, Anyway?
Scleroderma is a group of autoimmune diseases that can bring about changes to the skin, blood vessels, muscles, and even internal organs. It is a rare rheumatic disease that affects connective tissue and the vascular system. This condition makes the body produce too much collagen, which is a protein that usually adds strength to organs and tissues. Basically, it causes hardening of connective tissue, and that's a big part of what it does.
The disease is ongoing, or chronic, and it causes an abnormal growth of connective tissue. It can affect the joints, the skin, and internal organs, and it typically gets worse over time. Learning about the types, causes, risk factors, and symptoms is a good first step, you know, for anyone wanting to understand this condition better.
The Autoimmune Connection
As an autoimmune disease, scleroderma involves the immune system behaving in an unusual way. Instead of just fighting off bad germs, the immune response tricks tissues into causing inflammation and fibrosis, which is a thickening, in the skin and other parts of the body. This is why it's so important to recognize that it's a condition where your own body's defenses are involved, in a way.
The Many Faces of Scleroderma Skin Changes
While people often ask about a "scleroderma rash," what they are usually thinking of are the distinct skin changes that occur. Scleroderma causes areas of tight, hard skin. These aren't typically red, bumpy rashes, but rather alterations in the skin's texture, thickness, and sometimes color. These changes can look quite different from person to person, and sometimes, they can be subtle at first, just a little bit different.
Early Signs on Your Skin
Sometimes, the very first signs of scleroderma on the skin can be swelling or puffiness, especially in the fingers and hands. People might also notice changes in their hands and feet in response to cold or stress, a phenomenon called Raynaud's. This involves blood vessels in the fingers and toes constricting, causing them to turn white, then blue, and then red as blood flow returns. It's a common early sign, and quite noticeable, really.
Other early skin signs might include patches that feel different to the touch, or areas that seem to have lost some elasticity. There can be a feeling of tightness, even before visible hardening. It's important to pay attention to these subtle shifts in how your skin feels, as they can be quite telling, in fact.
Skin Thickening and Hardening
The most defining characteristic of scleroderma's effect on the skin is its thickening and hardening. The provided information mentions that scleroderma causes "parches de piel dura y gruesa," which translates to patches of hard and thick skin. This happens because of that excessive collagen production we talked about. The skin can become shiny, smooth, and feel very taut, almost like it's stretched too tight over the body.
This hardening can make it difficult to move joints, especially in the fingers, hands, and face. It can limit range of motion and make everyday tasks challenging. For instance, bending fingers or opening the mouth wide might become harder. This is a significant aspect of the condition, and it's something that can impact daily life quite a bit, you know.
Color Changes and Discoloration
Skin affected by scleroderma can also show changes in color. Some people might develop areas of darker skin, known as hyperpigmentation, while others might see lighter patches, called hypopigmentation. These color shifts can sometimes create a mottled or patchy appearance. Tiny, dilated blood vessels, called telangiectasias or spider veins, can also appear on the skin, often on the face, chest, or hands. These are typically small red spots that don't go away with pressure, and they are pretty common, as a matter of fact.
Other Skin Concerns
Beyond thickening and color changes, scleroderma can lead to other skin issues. Dryness is a common complaint, especially in the mouth and eyes, because the disease can affect the glands that make moisture. This can make the skin feel rough and uncomfortable. Sores or ulcers, particularly on the fingertips, can also develop due to poor blood flow to the skin, which is a concern for many. Sometimes, small, hard calcium deposits, called calcinosis, can form under the skin, especially around joints or pressure points. These can sometimes be painful or break through the skin, and that's something to watch for.
Why Does Scleroderma Affect the Skin?
The reason scleroderma affects the skin so profoundly goes back to its core mechanisms: the overproduction of collagen and issues with blood vessels. These two factors work together to create the visible skin changes. It's a complex interplay, and it's quite fascinating, really, how the body can react this way.
Collagen Overproduction
The primary reason for the skin's hardening is the excessive production of collagen. Collagen is a normal and necessary protein in the body, providing structure and strength to connective tissues. However, in scleroderma, the body produces too much of it, and it's laid down in an abnormal way. This extra collagen builds up in the skin, making it thick, stiff, and less flexible. This process is called fibrosis, and it's essentially what causes the skin to feel tight and hard. It's like the body is trying to over-repair itself, but in a way that causes problems.
Blood Vessel Involvement
Scleroderma can also harm your blood vessels. This damage to the vascular system plays a significant role in the skin changes. When blood vessels are affected, blood flow to the skin can be reduced, which can lead to the color changes, dryness, and even sores we discussed. The impaired blood flow also contributes to the overall health of the skin, making it more vulnerable. This connection between blood vessels and skin health is pretty important, you know, for understanding the full picture.
Localized vs. Systemic Scleroderma: Skin Differences
Scleroderma is not just one disease; it's a group of conditions. The way it affects the skin can depend on whether it's localized scleroderma or systemic sclerosis. This distinction is quite important for diagnosis and treatment, and it's something doctors look at very carefully.
Localized Scleroderma: Morphea and Linear Scleroderma
Localized scleroderma primarily affects the skin and sometimes the tissues just beneath it, like fat or muscle. It typically does not involve internal organs. The provided information notes that "the disease can be either localized to the skin." The two main types are morphea and linear scleroderma.
Morphea: This type appears as waxy, oval-shaped patches on the skin. These patches can be lighter or darker than the surrounding skin, and they can feel hard or firm. Morphea patches can vary in size and number, and they might appear on the trunk, limbs, or face. They usually do not spread to other parts of the body, and they often soften over time, though some discoloration might remain. It's more of a cosmetic concern for many, though it can impact mobility if it crosses a joint, basically.
Linear Scleroderma: This type appears as a single line or band of hardened skin, often on an arm, leg, or the forehead. When it occurs on the forehead, it's sometimes called "en coup de sabre," meaning "saber cut," because of its appearance. Linear scleroderma can affect not just the skin but also the underlying bone and muscle, potentially leading to limb length differences or joint contractures in children. It's a more serious form of localized scleroderma, in some respects.
Systemic Scleroderma: Diffuse and Limited
Systemic sclerosis (SS) is an autoimmune disorder that causes atypical growth of connective tissues. Unlike localized scleroderma, systemic sclerosis can affect not only the skin but also internal organs like the lungs, heart, kidneys, and digestive tract. "Scleroderma usually affects your skin, but can cause symptoms in" other areas. This form is considered an ongoing and degenerative disease that can get worse over time. There are two main subtypes:
Limited Cutaneous Systemic Sclerosis: In this type, skin thickening is usually limited to the fingers, hands, forearms, feet, and face. People with limited systemic sclerosis often experience Raynaud's phenomenon for many years before other symptoms appear. They might also develop telangiectasias and calcinosis. While skin involvement is less widespread, internal organ involvement can still occur, but it tends to develop later and is often less severe than in the diffuse form. It's a bit slower moving, you could say.
Diffuse Cutaneous Systemic Sclerosis: This is a more widespread form where skin thickening can occur on the trunk, upper arms, and thighs, in addition to the areas affected in limited scleroderma. Internal organ involvement tends to happen earlier and can be more severe in diffuse systemic sclerosis. The disease can affect the joints, skin, and internal organs, and it's typically more aggressive. This form usually requires more intensive monitoring and treatment, as a matter of fact.
Getting a Diagnosis: When to See a Doctor
If you notice persistent skin changes, especially hardening, swelling, or color changes that don't go away, it's a good idea to see a doctor. Early diagnosis can be very helpful in managing scleroderma and preventing potential complications. The exact cause of scleroderma is unknown, but understanding its manifestations is key for diagnosis. So, getting medical advice is pretty important.
The Diagnostic Journey
Diagnosing scleroderma involves a careful look at your symptoms, a physical examination, and various tests. A doctor will check your skin for changes in texture and thickness. Blood tests can look for specific antibodies that are often present in people with scleroderma. Sometimes, a skin biopsy, where a small piece of skin is removed for examination under a microscope, can help confirm the diagnosis. This whole process helps piece together the puzzle, basically.
Team Effort in Care
Diagnosing and treating scleroderma truly requires a team effort involving you and several types of health care professionals. Internists, who specialize in diagnosis, are often the first point of contact. You might also see a rheumatologist, a doctor who specializes in autoimmune and rheumatic diseases, or a dermatologist, who specializes in skin conditions. Other specialists, like pulmonologists for lung involvement or gastroenterologists for digestive issues, might also be part of your care team. This multidisciplinary approach ensures all aspects of the disease are addressed, which is really quite helpful.
Living with Scleroderma Skin Changes: Tips and Support
Living with scleroderma skin changes can be challenging, but there are many ways to manage symptoms and improve your quality of life. Research is finding better ways to treat symptoms, prevent organ damage, and improve the quality of life for people with scleroderma. These tips can help you take an active role in your care, and that's something to feel good about.
Managing Skin Symptoms
Moisturize Regularly: Keeping your skin well-hydrated can help with dryness and discomfort. Use thick, emollient creams or oint daily, especially after bathing. This helps maintain skin barrier function, and it's a simple step that can make a big difference.
Gentle Skin Care: Avoid harsh soaps, hot water, and vigorous scrubbing, which can irritate already sensitive skin. Opt for mild, fragrance-free cleansers. Treat your skin gently, as it's already working hard, you know.
Physical Therapy: If skin hardening affects your joints, physical or occupational therapy can be very beneficial. Therapists can teach you exercises and stretches to maintain flexibility and range of motion. This can help prevent contractures and keep you moving, in a way.
Protect from Trauma: Be mindful of cuts, scrapes, or pressure on the skin, as these can be slow to heal. Wear protective gloves for household chores or gardening. Small injuries can become bigger problems, so it's best to be careful, as a matter of fact.
Protecting Your Skin
Sun protection is very important for people with scleroderma, as sun exposure can sometimes worsen skin discoloration. Use broad-spectrum sunscreen with a high SPF, wear protective clothing, and seek shade when outdoors. Protecting your skin from the elements is a simple yet very effective strategy for managing its health, and it's something you can do every day.
Emotional Well-being
Dealing with a chronic condition like scleroderma, especially when it affects your appearance, can take a toll on your emotional health. It's important to acknowledge these feelings and seek support. Connecting with others who have scleroderma through support groups can be incredibly helpful. Talking to a counselor or therapist can also provide strategies for coping. Your mental health is just as important as your physical health, and that's something to remember, truly.
The Future of Scleroderma Research and Treatment
The good news is that research into scleroderma is ongoing and making strides. Multidisciplinary research has provided new clues for understanding this complex disease. Programs support basic, translational, observational, and clinical studies on scleroderma, fibrosis, and autoinflammatory diseases. This work is all about finding better ways to treat symptoms, prevent organ damage, and improve the quality of life for people living with scleroderma. For instance, there are labs focused on scleroderma genomics and health disparities, which is pretty exciting.
Translational research programs are working to bridge the gap between laboratory discoveries and patient care, aiming to bring new treatments to those who need them. This dedication to understanding the disease at a fundamental level and translating that knowledge into practical solutions offers real hope for the future. You can learn more about ongoing research efforts by visiting organizations like the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) at https://www.niams.nih.gov/health-topics/scleroderma, which is a great resource, by the way.
Frequently Asked Questions About Scleroderma Skin
What does scleroderma skin look like?
Scleroderma skin often looks tight, shiny, and thickened. It can feel hard or waxy to the touch. You might see patches that are lighter or darker than your usual skin tone, or small red spots from widened blood vessels. In some cases, there might be swelling, especially in the hands and feet. It's not usually a red, bumpy rash, but rather a change in texture and appearance, basically.
Is scleroderma rash itchy?
/Scleroderma-resized-56aae71e5f9b58b7d0091456.jpg)

Detail Author 👤:
- Name : Ms. Kallie Prohaska
- Username : glover.pierce
- Email : zieme.howell@nicolas.biz
- Birthdate : 1984-12-14
- Address : 463 Casper Point Shanahanhaven, MO 34550
- Phone : 678-234-8055
- Company : Volkman-O'Hara
- Job : Scanner Operator
- Bio : Dolores quibusdam iste odit. Voluptas odit atque deserunt et aut qui. Ipsam cupiditate fugit tempore maxime. Dicta reprehenderit aut ipsa nobis amet placeat.
Socials 🌐
linkedin:
- url : https://linkedin.com/in/clarissakeebler
- username : clarissakeebler
- bio : Aut in ea in.
- followers : 821
- following : 761
tiktok:
- url : https://tiktok.com/@clarissa6189
- username : clarissa6189
- bio : Non quia quo magnam eos eum. Voluptas tempore vero nulla eos quia.
- followers : 3306
- following : 1077
instagram:
- url : https://instagram.com/keebler2015
- username : keebler2015
- bio : Quisquam provident illo voluptatum ut et delectus. Sed qui commodi rerum dicta.
- followers : 1814
- following : 2527
facebook:
- url : https://facebook.com/clarissa_keebler
- username : clarissa_keebler
- bio : Consequatur enim omnis ut ut pariatur libero.
- followers : 2379
- following : 330
twitter:
- url : https://twitter.com/clarissakeebler
- username : clarissakeebler
- bio : Animi dolores similique laborum qui laborum. Quaerat assumenda magnam laboriosam mollitia.
- followers : 3101
- following : 2309